A Basic Care Plan for Diabetes
–
We’ve looked at the causes and the risk factors of diabetes.
We’ve even gone through the signs, symptoms and conditions associated with diabetes.
But as a nurse, how would you apply this knowledge to the short-term, and long-term care of your patients?
What is the Expected Nursing Outcome for Diabetes?
One of the first things you need to ask yourself when thinking of a care plan for your patient is ‘What is the Expected Outcome?’
What is the goal that needs to be set to deal with the presenting condition?
For diabetes, the ultimate outcome will always be to:
“Achieve and maintain glycaemic control within the correctly identified ranges and continuous blood glucose monitoring.”
Nursing Assessment
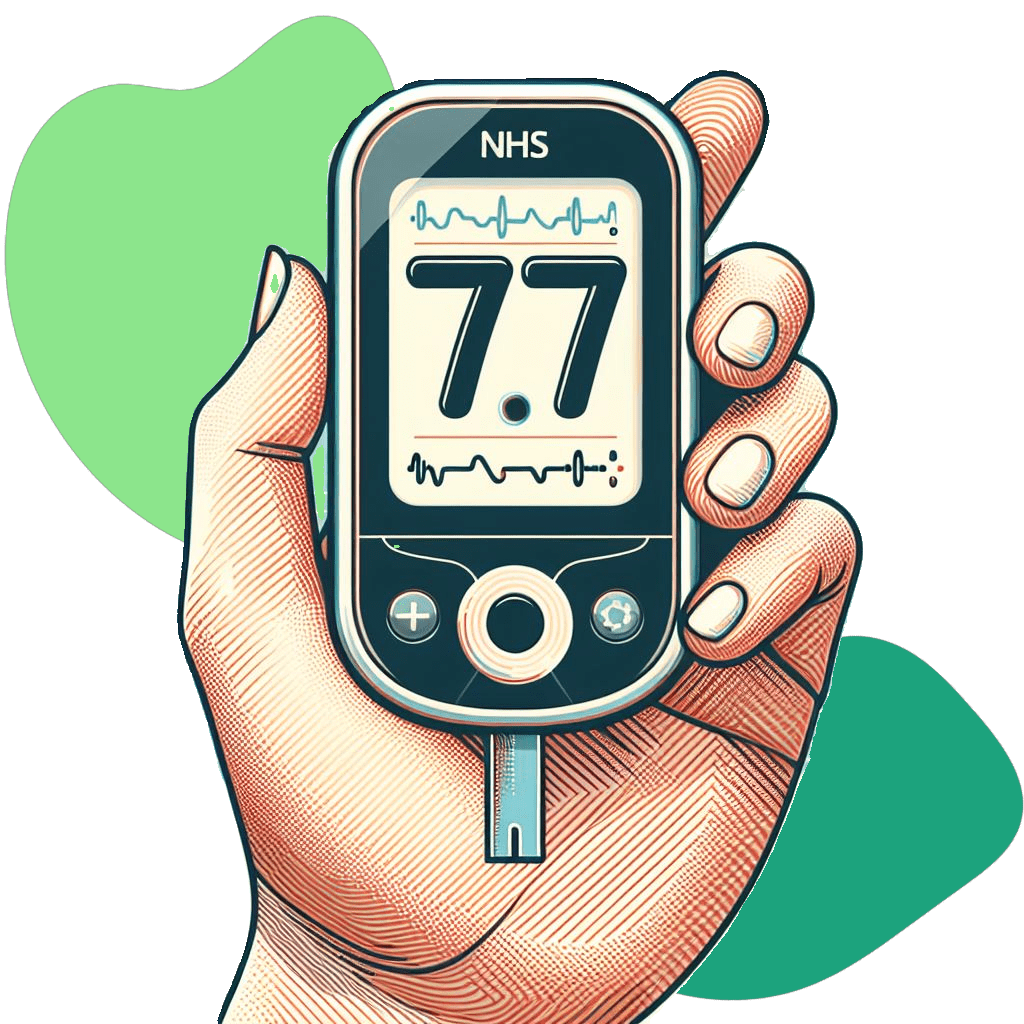
The main, and most basic, nursing assessment that should be done for a diabetic patient should be to monitor their blood glucose levels.
You can use a blood glucose meter to check their levels before and after meals, at bedtime, and whenever they feel unwell.
This should be done in regular intervals (usually just before a meal), and even more often if your patient is on a Variable Rate Intravenous Insulin Infusion (VRIII) – previously known as a sliding scale.
And in the case of a patient with Diabetic Ketoacidosis (DKA), as part of the nursing assessment, you will also need be monitoring their ketone levels.
Document these blood glucose levels, as well as your patient’s medication adherence according to local policy.
✾ A nursing assessment that may sometimes be missed is to carry out a regular assessment of your patient’s skin.
This will especially contribute towards the nursing care of a diabetic patient with neuropathy, as these patients are prone to unrecognised injuries on their feet.
Nursing Interventions
Looking back at the main nursing outcome for a diabetic care plan creates the question of ‘How?’.
Most people can carry out the necessary assessments, but how do you apply this to your patients care the proper way?
It can be brought down to a few points:
Prevent hyperglycaemia (high blood glucose) and hypoglycaemia (low blood glucose):
Hypoglycaemia is when the blood glucose level is too low, usually below 4 mmol/L. It can cause symptoms such as sweating, shaking, dizziness, confusion and even loss of consciousness.
Hyperglycaemia is when the blood glucose level is too high, usually above 11 mmol/L. It can cause symptoms such as thirst, dry mouth, frequent urination, blurred vision, fatigue, headache, nausea or fruity breath.
Preventing and treating complications and conditions related to diabetes:
Although the main outcome for diabetes, as a whole, is focused on maintaining glycaemic control, there are additional nursing aspects of care that consider a much wider range of factors.
This includes the prevention and treatment of complications that are acute and life-threatening, such as diabetic ketoacidosis (DKA), which is a condition where the body produces too many ketones, which are acidic substances that can poison the blood and organs.
Other complications are chronic and progressive, such as cardiovascular diseases, diabetic retinopathy, chronic kidney disease, infection and neuropathies, which can damage the heart, blood vessels, eyes, kidneys, skin and nerves.
These can cause problems such as heart attack, stroke, blindness, kidney failure, amputation and disability.
To manage these key points, and take charge of your plan, you will need to focus on the following:
Assess your patients’ blood glucose levels regularly and escalate any concerns when necessary.
You should aim to keep their blood glucose levels within the target range recommended by their doctor or diabetes care team.
Learn about the different types of insulin and how to use them safely and effectively.
Know the benefits and risks of each type of insulin, such as rapid-acting, short-acting, intermediate-acting, long-acting and mixed insulins.
Know how to store, prepare and inject insulin correctly using the appropriate devices and techniques, such as syringes, pens or pumps.
It is important to rotate your patient’s injection sites, such as the abdomen, thighs or arms to prevent problems such as lipohypertrophy, which is characterised by stiff, lumpy skin and can result in inconsistent absorption of the insulin.
Oral antidiabetic agents are pills that help lower blood glucose levels in people with type 2 diabetes who still produce some insulin.
They work by different mechanisms, such as stimulating the pancreas to produce more insulin, reducing the liver’s glucose production, improving the cells’ insulin sensitivity or slowing down the digestion of carbohydrates.
As a nurse, you should help them follow their medication regimen as prescribed and encourage them not to refuse doses.
By having the knowledge and being able to explain the benefits of your patient taking their antihyperglycaemic medication (and the risks of not taking it), it will give your patient confidence in your nursing care.
You may need to manage the possible side effects of oral antidiabetic agents.
This includes stomach upset, weight gain or hypoglycaemia.
Help your patients manage these side effects by giving them some tips, such as eating small and frequent meals and drinking plenty of water.
Patients with diabetes can lose a lot of fluid and minerals from their body due to high blood sugar levels that make them urinate and drink more often.
This can affect their fluid, electrolyte, and acid-base balance, which is important for the normal functioning of their cells and organs.
If this balance is disturbed, it can cause problems such as weakness, confusion, irregular heartbeat and can even lead to a coma.
Therefore, you should monitor and record the patient’s fluid balance, address any concerns you have to the medical team and give them fluids or electrolytes as prescribed.
Patients with diabetes may experience pain and discomfort due to various causes, such as neuropathy, foot ulcers or infection.
Pain and discomfort can affect the patient’s mood, sleep, appetite and overall quality of life.
Therefore, nurses should assess the patient’s pain and discomfort level and provide appropriate relief and comfort measures. Some of the ways to manage pain and discomfort include:
- Using a pain scale, such as the numerical rating scale (NRS) or the faces pain scale (FPS), to measure the intensity and location of the pain and discomfort.
- Giving the patient analgesics as prescribed.
- Applying non-pharmacological methods, such as heat, cold or distraction to reduce the pain and discomfort.
- Encouraging the patient to report any changes or problems with their pain and discomfort.
People with diabetes are more likely to develop foot problems, such as ulcers or infections (which may lead to amputations), because of the damage that high blood glucose levels can cause to the nerves and blood vessels in the feet.
Nursing care should include:
Inspect your patients’ feet every shift for any problems, such as cracks, sores, corns, calluses or nail problems.
Help your patients wash their feet with warm water and soap. Dry them gently, especially between the toes.
Apply a thin layer of moisturizer to keep the skin soft and prevent cracking BUT avoid putting moisturizer between the toes as this can cause fungal infection.
You can also advise your patients to trim their toenails (straight across and file the edges with a nail file, whilst avoiding cutting the nails too short or digging into the corners, as this can cause ingrown toenails or infection).
If they have trouble cutting their nails, or you do not feel confident to do it correctly, then you can and should make a referral to a podiatrist as they will have much more training in this area.
Encourage your patients to wear comfortable, well-fitting shoes and socks that protect their feet and allow them to breathe.
Shoes that are too tight, too loose, or have seams or rough edges can rub or cause blisters, and should be avoided.
They should avoid wearing sandals, flip-flops and walking around with their bare feet, as these can expose their feet to injury or infection.
Their shoes and socks should be checked for any objects, such as stones, nails or pins, that can hurt their feet.
If possible, you should ask a patient’s relatives to bring this suitable footwear in.
Patients with diabetes are more prone to developing wounds, especially in the feet, due to the damage that high blood glucose levels can cause to the nerves and blood vessels.
Wounds can impair the patient’s mobility and increase the risk of infection and amputation.
Therefore, nurses should promote wound healing and prevention by doing these things:
- Inspecting the patient’s feet and other areas of the body for any signs of wounds, such as cuts, blisters, sores or ulcers and escalating when necessary.
- Cleaning and dressing the wounds properly and regularly, using aseptic technique and the appropriate dressings.
- Monitoring the wound healing process and looking for any signs of infection, such as redness, swelling, pain, or pus and treating them promptly with antibiotics or other medications as prescribed.
- Educating the patient and the family about the importance of wound care and prevention, and how to do it at home, such as by keeping the wounds clean and dry, changing the dressings as instructed, and avoiding pressure or friction on the wounds.
People with diabetes may experience various emotions and stress related to their condition, such as anger, sadness, fear, guilt or frustration.
These can affect their mood, self-esteem and well-being, which could make it harder for them to manage their diabetes for themselves.
You can help your patients with diabetes cope with their emotions and stress by providing them with emotional support:
- Listen to your patients and empathize with their feelings
- Avoid judging, criticizing, or blaming them for their condition or their actions. Instead, offer them encouragement, praise and positive feedback for their efforts and achievements
- Teach your patients how to cope with stress and relax. Stress can worsen their blood glucose control and affect their physical and mental health.
- Help them recognize the sources and signs of stress in their life and find ways to reduce or manage their stress, such as planning, prioritizing, delegating or simply by saying no.
- Teach them relaxation techniques, such as breathing, meditation or yoga.
- Encourage them to do something they enjoy, such as reading, gardening or playing games.
- Support your patients in building and maintaining a strong social network.
- Having a good support system can help them cope with their diabetes and improve their well-being.
- Help them involve their family, friends and even co-workers in their diabetes care, such as by educating them about their condition or asking for their help.
- Help them find and access community resources, such as diabetes educators, counsellors, or social workers.
Patients with diabetes need a team approach to get the best care possible.
You should work closely with the primary care providers and specialists who are involved in the patient’s diabetes care, such as the diabetic nurse, doctors, dietitians, pharmacists or podiatrists.
You should communicate with them regularly, share information, and coordinate care plans.
This way, you can ensure that the patient gets comprehensive and consistent care for their diabetes and any related conditions.
✾ Humulin, the first insulin made from human cells, was invented by scientists in 1978. This insulin has the same structure as the insulin that the human body makes.
Things to Consider When Caring for a Diabetic Patient
Each patient’s situation will be different, so it would be your job to tailor the diabetic care plan to suit each individual.
Here are some of the things you may need to consider:
Make sure you are well-trained and educated on how to provide adequate nutrition to patients with diabetes who need NG or PEG feeding.
You should know the type, amount and timing of the feed, as well as how to monitor and adjust it according to the patient’s blood glucose levels and needs.
Prevent and treat any infections that may affect the patient’s nutrition and glucose control, such as gastroenteritis, by following the infection prevention and control guidelines, such as washing your hands, wearing gloves and aprons, and cleaning and disinfecting the equipment and the environment.
You should also monitor the patient for any signs and symptoms of infection, such as fever, diarrhoea, vomiting, or abdominal pain and escalate if necessary.
Chances are that if you have a diabetic patient who is NBM, they will be put on the variable rate intravenous insulin infusion (VRIII) protocol.
This protocol is used to maintain the patient’s blood glucose levels within the target range of 5-10 mmol/L, by giving them a continuous infusion of insulin and glucose.
You should follow the protocol carefully and adjust the insulin and glucose rates according to the patient’s blood glucose levels, which will usually be checked hourly.
When caring for a confused diabetic patient, regular mental status assessments are crucial.
Providing a safe environment and having strategies to manage behavioural disturbances are also important. Effective communication with the healthcare team and family members is key.
For patients with a language barrier, it’s helpful to use simple, non-medical language and visual aids to communicate with your patient about their diabetes.
Translation services can be utilized if available, and cultural differences should be considered.
In the case of a non-compliant patient, it’s important to identify and address barriers to compliance (which usually is related to a lack of understanding).
Education about the importance of medication compliance and the consequences of noncompliance can definitely be beneficial.
Providing support and resources to help the patient overcome barriers to compliance, along with regular follow-up to monitor progress can also be helpful.

If you come across a patient who has a complex care plan, don’t stress in silence. When in doubt, ask someone to help you out.
Patient Education in Diabetes Management
Diabetes management is a lifelong process that requires the involvement and commitment of the person with diabetes and their care team.
If a patient can only rely on others to provide care for their diabetes, then the long-term risk of mismanagement and future complications increases significantly.
As a nurse, you can help your patients with diabetes manage their condition by providing them with patient education on diabetes management.
What Should Your Patients Be Taught About Diabetes?
Nurses need to know the basics about a wide range of conditions, but a patient will only really need to know about their own.
This means that everything you should know, they should know too.
Take each aspect of your diabetic nursing care plan and find a way to transform it into a suitable piece of learning that your patient can take away with them.
For example, whilst administering insulin injections for your patient, you can explain them step-by-step what you are doing and even test their knowledge (such as asking them about the rotation of injection sites).
Even better, you should use your own judgement and could allow your patient to self-administer the insulin injection.
This promotes independence and gives them the confidence to carry this task out by themselves, without having to rely on others.
This form of educating your patients can apply to many aspects of diabetic care including medication management, self-hygiene, wound care, nutritional balance and weight management.
Addressing Challenges in Self-Management
You should always assess your patient’s motivation to learn and tailor your education to their needs, preferences and goals.
Doing this helps your patient to retain the information they are taught, rather than you both going through a never-ending cycle of confusion and frustration.
You can use various tools and methods to assess their readiness to learn, such as asking open-ended questions or using motivational language.
Try use different formats and materials to deliver your education, such as verbal, written, visual or interactive.
You can also involve your patients in setting their own goals and action plans and provide them with feedback and reinforcement.
Your Patient’s Ability to Learn:
Consider the specific needs and challenges of different age groups, such as children and older adults.
Children and older adults with diabetes may have different learning styles, cognitive abilities, physical limitations, emotional issues and social support than other age groups.
You can adapt your education to their developmental stage, functional status, mental capacity and cultural background.
You can also involve their family, caregivers or peers in their education and care.
Some patients may find it hard to manage their condition, especially if they are older or have other conditions that affect their memory, mobility or mood.
You should provide support and resources to help these patients manage their diabetes effectively.
This could be done by teaching them how to use devices, apps or reminders, involving their family or caregivers or referring them to support groups or programs.
✾ You will undoubtedly come across a few patients who will refuse their medication or neglect their own care.
✾ It might be frustrating at the time, but usually there is a reason. So, be patient and maybe even try to find out why.
So there you have it.
The nursing assessments and interventions that can be included in a care plan for your patient with diabetes, including a way that helps to promote their independence.
With this, you should be able to come across a diabetic patient and create a care plan that is perfect for them.
Question Time
Read the questions and if you have the answers, flaunt your knowledge and share your thoughts and experiences in the comment section below.
What are some of the latest trends and innovations in diabetes care that you find exciting or useful?
How do you educate and empower patients with diabetes to take an active role in their care and prevent complications?
What are some of the best practices and resources that you use to provide effective and person-centred care for patients with diabetes?