Subcutaneous Injection: The Basics
–
Ward nurses. Community nurses. Student nurses. Most other nurses you can think of.
If you have ever been part of a patient’s direct clinical care then you are, without a doubt, no stranger to subcutaneous injections.
So, how can you be sure that you are carrying out this common skill correctly?
Subcutaneous injections are not just about poking a needle into someone’s skin.
There is a risk to your patient if not done correctly, so you need to be sure that you know all you need to know.
What is a Subcutaneous Injection?
A subcutaneous injection is a way of delivering medication directly to the fat layer under the skin.
This layer is called the subcutaneous tissue, and it’s where you store all your extra calories and energy.
Subcutaneous injections are different from other types of injections, such as intramuscular (into the muscle) or intravenous (into the vein).
Subcutaneous injections are slower and gentler, because they don’t need to go through the muscle or the bloodstream.
✾ The term “subcutaneous” comes from Latin words ‘sub’ meaning “under” and ‘cutis’ meaning “skin,” hence subcutaneous injections are administered into the layer of skin directly below the dermis and epidermis, also known as the subcutis or the hypodermis.
Why are Subcutaneous Injections Necessary?
Some medications work best when they are injected into the fat layer because they need to be absorbed at a steady pace.
For example, insulin is a hormone that helps control blood sugar levels, and it needs to be injected into the fat layer to mimic the natural release of insulin from the pancreas.
Other medications that are given subcutaneously include growth hormone, octreotide, glucagon, and epinephrine.
Subcutaneous injections can also be helpful for patients who have trouble swallowing pills, or who have problems with absorbing or metabolising oral medications.
This form of injections can also reduce the risk of infection or irritation that may happen with other routes of medication.
✾ Subcutaneous injections are generally safer than intravenous and intramuscular routes. They are less likely to cause complications such as infections, nerve damage or injection into a blood vessel.
When to Perform a Subcutaneous Injection?
The timing and frequency of subcutaneous injections depend on the medication, the patient’s condition and the doctor’s prescription.
Some medications need to be given every day, while others may be given once a week or once a month.
And some need to be given at specific times of the day, such as before meals or at bedtime.
There are also medications that need to be given in relation to blood tests or other monitoring procedures.
It is very important to follow the instructions on the medication label and the prescription carefully, and to ask the doctor or pharmacist if you have any questions or doubts.
✾ Timing can be crucial when it comes to subcutaneous injections. For instance, insulin injections are often timed around meals, with the exact timing depending on the type of insulin and the individual’s specific needs.
✾ It’s also recommended to administer these injections at the same time each day to help keep blood sugar levels stable.
Step-By-Step: How to Perform a Subcutaneous Injection
Before you give a subcutaneous injection, you need to gather the following equipment:
Syringe
A syringe with a needle that is suitable for subcutaneous injection. The needle size depends on how big or small your patient is and how much fat they have under their skin. Generally, subcutaneous needles range from 25-31 gauge.

Bottle or Ampoule of Medication
A bottle or ampoule of medication that is prescribed for subcutaneous injection. Some injectable medications come pre-packed which means that you can skip all the hassle, but make sure to check the rights of medication before using it.

Sharps Bin
For throwing away used needles and syringes. And carrying the sharps bin with you isn't always the best option, so at least locate it before you start.
Gloves
For protecting your hands from germs and adhering to infection control protocol.
The steps for giving a subcutaneous injection are as follows:
- Wash your hands with soap and water or use an alcohol-based hand rub.
- Put on gloves, in adherence to infection control and local policy.
- Check the rights of medication administration (however many there are now)!
- Explain what you are going to do to the patient and get their consent.
- Choose a suitable spot for injection on the patient’s body – asking them where they prefer won’t hurt!
- Take off the needle cap and hold the syringe like a pencil or a dart in your main hand.
- Pinch up a fold of skin at the injection spot with your other hand – Remember, you are supposed to be separating the skin and fat from the muscle underneath.
- Put in the needle quickly and firmly at a 45° angle.
- Inject the medication slowly and smoothly by pushing the plunger all the way down.
- Pull out the needle swiftly and apply gentle pressure to the injection spot with some gauze. Do not rub or massage the area as this may cause discomfort or affect the absorption of the medication.
- Throw away the used needle and syringe in a sharps bin right away after use. Do not put back or bend the needle, as this may cause a sharps injury.
- Take off your gloves and wash or gel your hands.
- Complete your documentation, including the date, time, area, medication name, dose, route, as well as any side effects or problems.
✾ The common spots for subcutaneous injection are:
- The stomach (except for 2 inches around the belly button)
- The upper arms (on the outer back side)
- The thighs (on the front outer side)
- The bum (on the upper outer corner)
✾ You should change the spots regularly to avoid hurting or irritating the same area repeatedly.
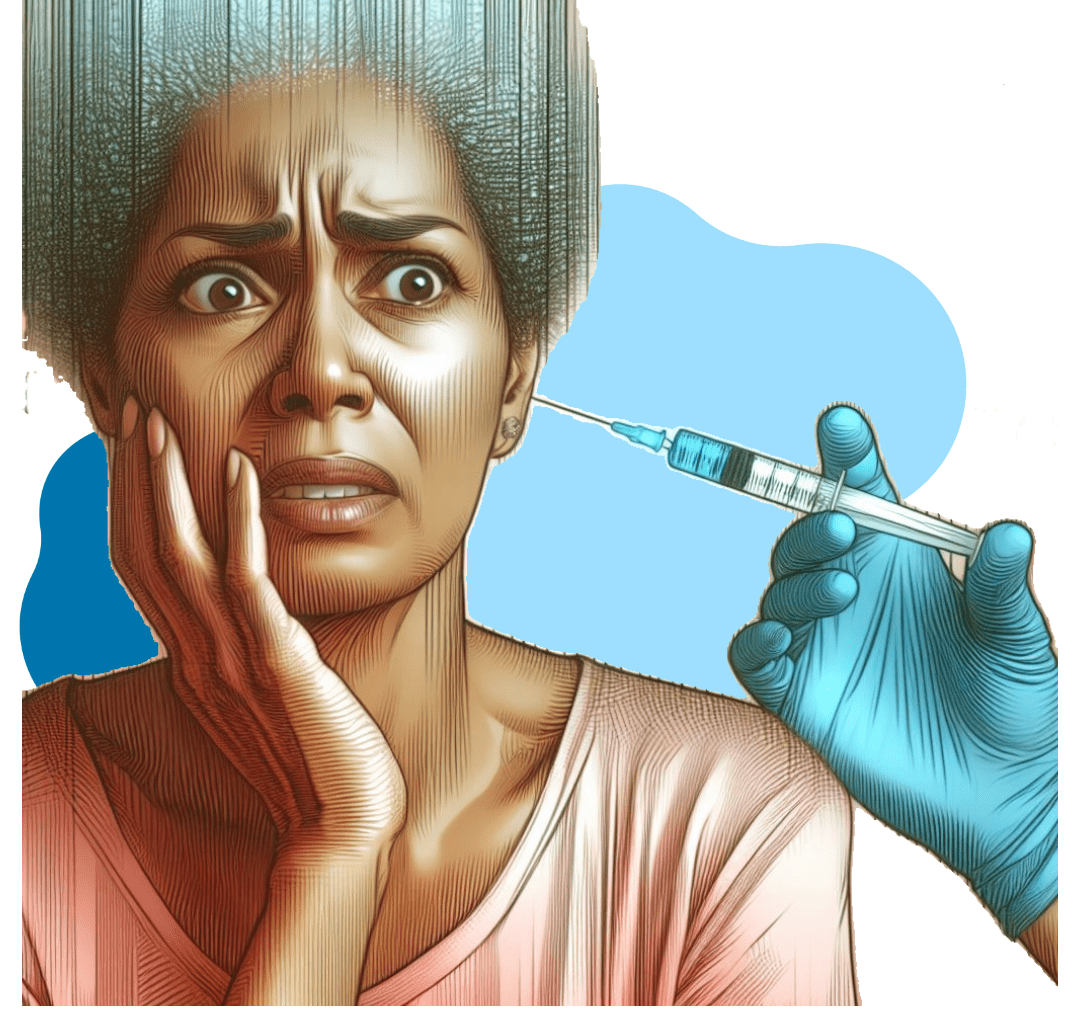
Rapid breathing? Sweating? Anxiety? These are all signs a person who has a needle phobia might display. So rather than waving a needle around, maybe try some distraction techniques instead!
What Happens When a Subcutaneous Injection is Not Done Correctly?
Although subcutaneous injections are a great way to deliver medications that need a steady and slow absorption into the bloodstream, whilst avoiding unwanted complications, it needs to be done accurately and with care.
Here are some of the things that could go wrong if you don’t follow the proper technique:
Pain
Nobody likes to feel pain, especially your patients. That’s why you should insert the needle gently and correctly, avoiding the sensitive nerve endings in the skin that can trigger a painful response.
Incorrect Absorption of Medication
The whole point of a subcutaneous injection is to ensure that the medication is absorbed at the right rate and amount. If you inject the medication too fast, too deep, or in the wrong place, you could compromise its effectiveness and put your patient at risk.
Infection or Irritation at the Injection Site
You should always clean the injection site with an alcohol pad and wait for it to dry before inserting the needle. You should also rotate the injection sites to prevent overuse and irritation of the same area.
Damage to Tissues
Subcutaneous injections are meant to go into the fatty layer under the skin, not into the muscle. If you insert the needle too deeply, you could damage the muscle tissues and cause bleeding, bruising, or inflammation.
✾ To prevent these complications, you should follow the steps above and use the correct technique when giving a subcutaneous injection. It’s as simple as that!
So there you have it.
Subcutaneous injections are a key skill for nurses, as they can give medications that are effective and convenient for patients.
They need careful preparation, technique and documentation to ensure safety and quality of care.
Question Time
Read the questions and if you have the answers, flaunt your knowledge and share your thoughts and experiences in the comment section below.
Do you remember giving your first subcutaneous injection? Or have you ever received a subcutaneous injection? What was your experience?
How do you cope with needle phobia or anxiety when giving or receiving subcutaneous injections?
What are some of the tips or tricks that you use to make subcutaneous injections easier or more comfortable?